Abstract
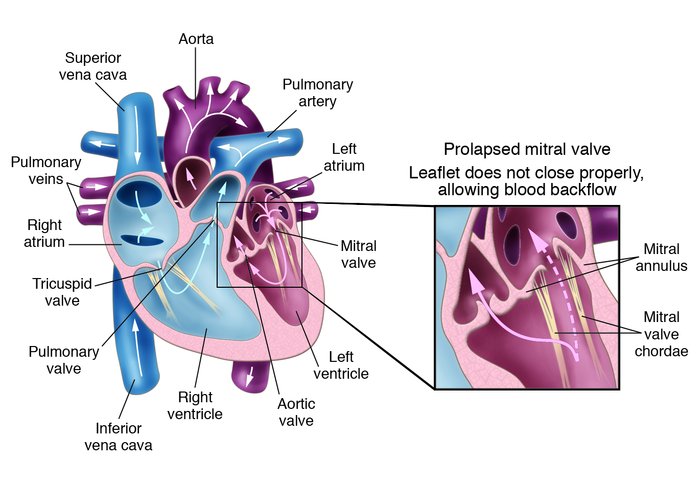
Mitral valve prolapse (MVP), an abnormal displacement into the left atrium of a thickened and redundant mitral valve during systole, is a relatively frequent abnormality in humans and may be associated with serious complications. A recent study implicates fibrillin-1, a component of extracellular matrix microfibrils, in the pathogenesis of a murine model of MVP. This investigation represents an initial step toward understanding the mechanisms involved in human MVP disease and the development of potential treatments.
Authors
Arthur E. Weyman, Marielle Scherrer-Crosbie
Figure 1
Options:
View larger image
(or click on image)
Download as PowerPoint
MVP. Mitral valve leaflets, shaped like parachutes, are attached to the inner wall of the left ventricle by a series of strings called chordae. When the ventricles contract, the mitral valve leaflets close snugly to prevent backflow of blood from the left ventricle into the left atrium. Upon ventricle relaxation, the valves open to allow oxygenated blood from the lungs to fill the left ventricle. In patients with MVP, myxomatous degeneration of the leaflets and chordae results in leaflet thickening and redundancy, causing the leaflets to prolapse, or flop backwards, into the left atrium (detail). This sometimes allows leakage of blood through the mitral valve (mitral regurgitation). Severe mitral regurgitation can lead to heart failure and abnormal heart rhythms.



Copyright © 2025 American Society for Clinical Investigation
ISSN: 0021-9738 (print), 1558-8238 (online)