Abstract
Harlequin ichthyosis (HI) — the most severe form of keratinizing disorders, often lethal in the neonatal period — is characterized by a profound thickening of the keratin skin layer, a dense “armor”-like scale that covers the body, and contraction abnormalities of the eyes, ears, and mouth. In this issue of the JCI, Akiyama et al. report that mutations in ABCA12 caused defective lipid transport that significantly impacted normal development of the skin barrier. Lipid secretion was recovered after corrective ABCA12 gene transfer into patient keratinocytes. These results should allow for early prenatal diagnosis of HI and lend hope to the possibility of a specific treatment for this devastating disorder.
Authors
Alain Hovnanian
Figure 1
Options:
View larger image
(or click on image)
Download as PowerPoint
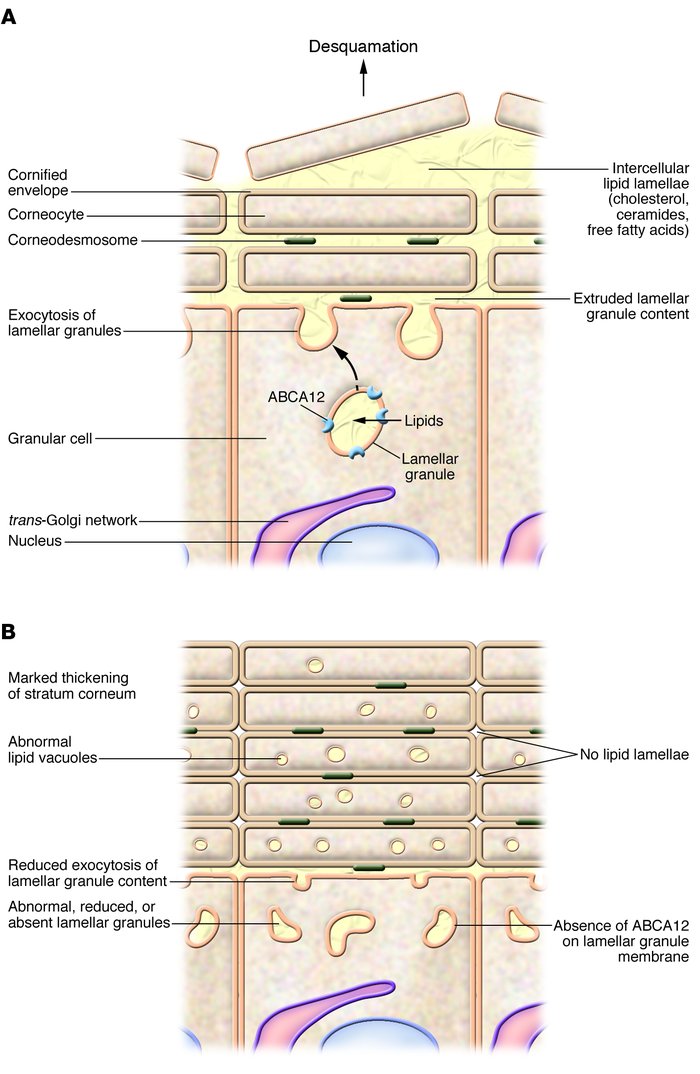
Mutations in lipid transporter ABCA12 cause HI. (A ) In the granular layers of healthy skin, the ABCA12 lipid transporter transfers lipids from the cytosol into lamellar granules where lipid-processing enzymes, proteases, and protease inhibitors are also concentrated. At the granular layer–stratum corneum interface, the lamellar granules fuse with the cell membrane and discharge their content into the intercellular lamellae. Complex enzymatic reactions lead to modifications of the lipid composition of the intercellular space (cholesterol, ceramides, free fatty acids) that provide a very effective water-permeability barrier. Corneocytes detach from each other in the superficial layers of the stratum corneum as a result of finely regulated proteolytic cleavage of corneodesmosomes. (B ) In the skin of HI patients, the absence of ABCA12 prevents the transfer of lipids into lamellar granules, which themselves are abnormally shaped, reduced in number, or absent. As a result, exocytosis of lamellar granule content is reduced and intercellular lipid lamellae are absent. Abnormal lipid-containing vacuoles form in the cytoplasm of the corneocytes. The stratum corneum is remarkably thickened and does not desquame.



Copyright © 2026 American Society for Clinical Investigation
ISSN: 0021-9738 (print), 1558-8238 (online)