Abstract
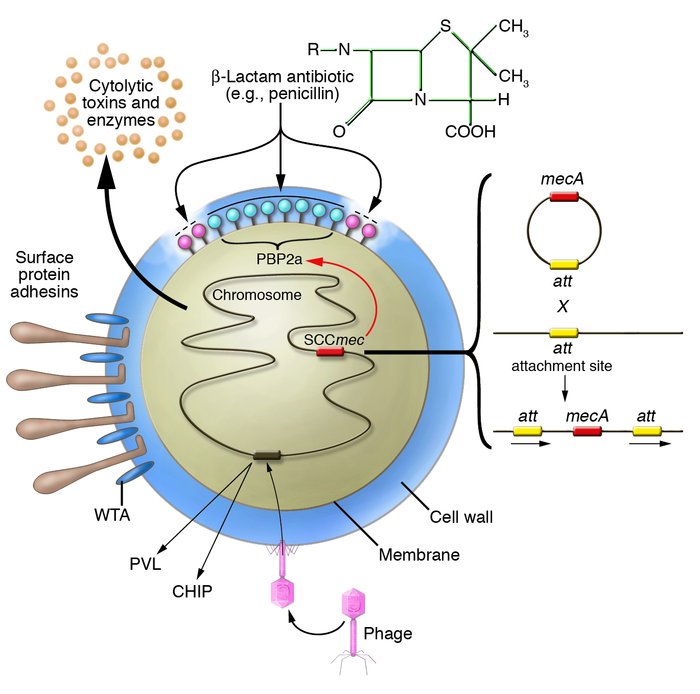
There has been some debate about the disease-invoking potential of Staphylococcus aureus strains and whether invasive disease is associated with particularly virulent genotypes, or “superbugs.” A study in this issue of the JCI describes the genotyping of a large collection of nonclinical, commensal S. aureus strains from healthy individuals in a Dutch population. Extensive study of their genetic relatedness by amplified restriction fragment typing and comparison with strains that are associated with different types of infections revealed that the S. aureus population is clonal and that some strains have enhanced virulence. This is discussed in the context of growing interest in the mechanisms of bacterial colonization, antibiotic resistance, and novel vaccines.
Authors
Timothy J. Foster
Figure 1



Copyright © 2026 American Society for Clinical Investigation
ISSN: 0021-9738 (print), 1558-8238 (online)